How a Hong Kong man’s drug-resistant Epilepsy was relieved using robotics
Neurosurgery expert says new approach could encourage more people to get check-ups for epilepsy conditions
Hongkonger Lo Wai-shing, 45, was diagnosed with drug-resistant epilepsy when he was 15 and says he once suffered from 10 seizures in a single month and might still experience one or two episodes a month despite taking medication.
Holding down a regular job proved difficult due to his condition, he said, adding that he had only ever worked for his uncle’s company and a supermarket that also employed his aunt.
Lo underwent minimally invasive surgery at Queen Mary Hospital in April that involved a new robotic system. The procedure allowed doctors to identify the area of his brain that was causing the seizures and use heat generated by radio waves to destroy a small part of the tissue to help relieve his condition.
“In the month after the surgery, I have not had any seizures, and I sleep very well,” he said. “I am very happy as it has largely reduced the frequency of the seizures.”
The new robotic system means doctors in Hong Kong can use a more accurate and less invasive approach to identify the sources of epilepsy conditions that are untreatable with medication.
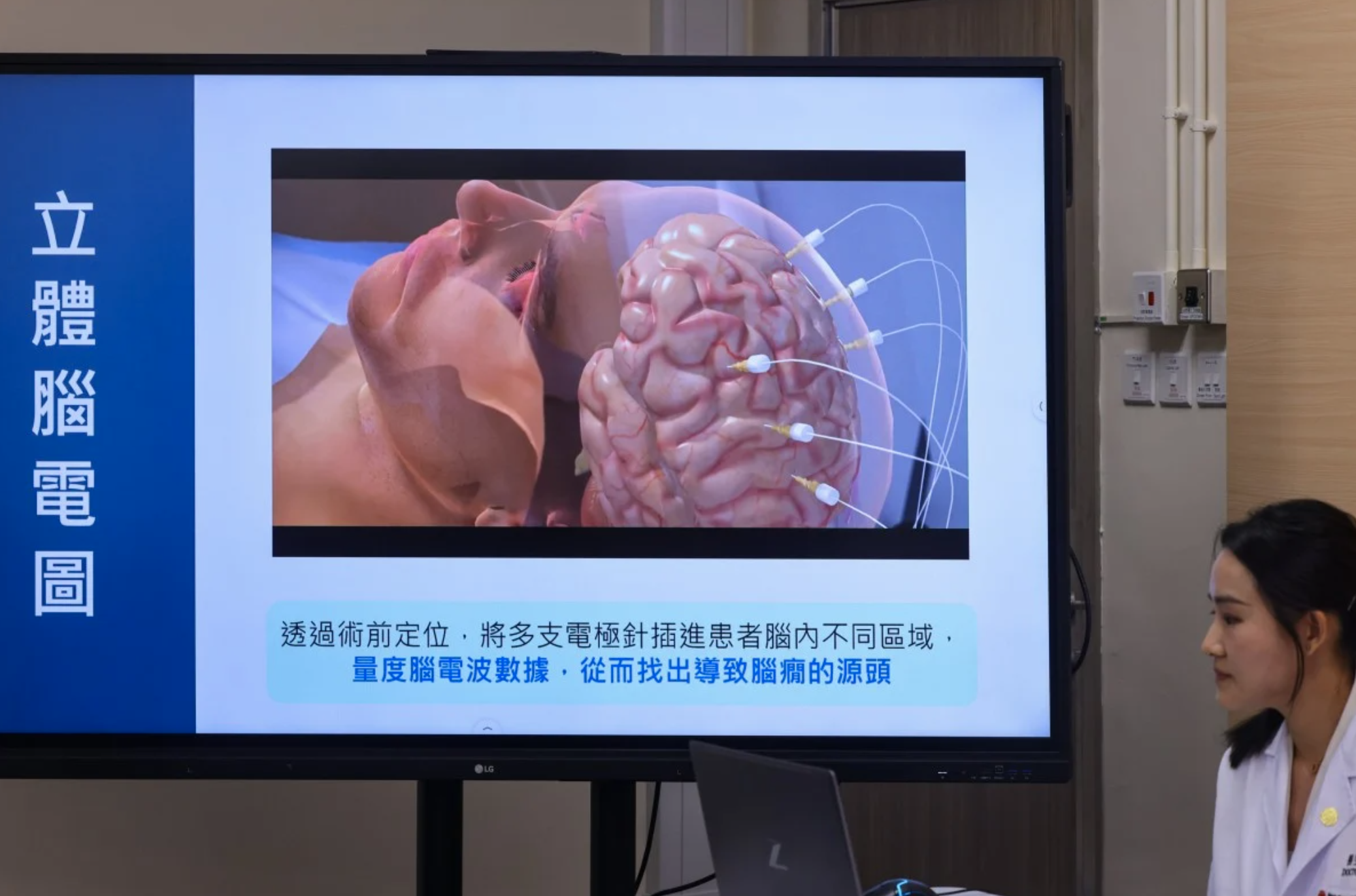
Dr Benedict Taw Beng-teck, a neurosurgery consultant at the hospital, said the system could assist surgeons during a procedure named stereoelectroencephalography (SEEG), which involves locating the area of the brain that causes epilepsy.
He said he hoped the new approach could encourage more people to get check-ups for such conditions.
The new process involves surgeons inserting more than a dozen needlelike wires, known as electrodes, all over a patient’s brain, with intricate calculations and measurements required to identify the correct locations and depths.
Without the system, doctors would have to use a technique called “frame-based stereotaxy”, which attaches a frame to the patient’s head to manually measure the angle and the depth of every electrode’s trajectory.
“It’s very time-consuming, and it’s prone to human error,” he said in a press briefing. “So the robotic system basically eliminates us having to adjust for every different trajectory and angle.”
(From left) Queen Mary Hospital’s Dr Lau Hoi-to, Dr Benedict Taw and Dr Ian Leung Yu-hin and epilepsy patient Lo Wai-shing discuss the impact of the new robotic system at a press event. Photo: Nora Tam
Taw said doctors would only need to input scans and images of the patient’s brain into the robotic system and select the target entry points.
“All we have to do is touch a button, press on a pedal, actually, and then [the robotic system] will guide us to the correct trajectory,” he said. “That saves a lot of time and is also very accurate, [and] eliminates human errors.”
Queen Mary Hospital said the new system was introduced in January last year and has assisted more than 10 cross-disciplinary surgical operations, including three involving epileptic patients and another two for people with movement disorders.
Taw said that about 60,000 to 70,000 people were estimated to be suffering from epilepsy, while one in 20 people would experience an epileptic episode in their lifetime.
Epilepsy is a chronic disease characterised by recurrent seizures, where the brain’s functions lose control.
The condition can lead to abnormal sensations and behaviours, muscle twitching and even loss of consciousness, significantly impacting a patient’s daily life and increasing the risk of injury or death.
Taw said that while epilepsy could typically be treated with medication, it might not work for about 30 per cent of patients, with doctors potentially recommending surgery to remove the area of the brain causing the condition.
Before the procedure could take place, doctors needed to conduct an SEEG to identify the area of the brain that needed to be removed.
Taw said before the frame-based stereotaxy was introduced, patients would need to undergo a craniotomy, which involved having their skull cut open, for an SEEG.
“In the past, a lot of patients didn’t want to undergo this kind of SEEG because of the invasive nature of the surgery,” he said.
“But now this robotic system is less invasive and [more accepted]. Hopefully, more patients will benefit from this procedure.”
Taw said that in Lo’s case, doctors had spent nearly 3½ hours implanting 15 electrodes into his brain, a process that used to take them about seven hours to do using the previous frame-based system.
Source: Sammy Hueng, https://www.scmp.com/news/hong-kong/health-environment/article/3316266/how-hong-kong-mans-drug-resistant-epilepsy-was-relieved-using-robotics